Regular use of common over-the-counter (OTC) medications containing diphenhydramine, a widely used antihistamine, may be linked to an increased risk of cognitive impairment, including dementia, according to recent studies and expert warnings. The drug, commonly found in sleep aids like Benadryl, Tylenol PM, and Unisom, as well as allergy medications, has raised concerns among healthcare professionals about its potential long-term effects on brain health, particularly in older adults.
Millions of Americans routinely turn to these readily available medications to alleviate allergy symptoms, insomnia, and cold-related issues. However, growing scientific evidence suggests that the anticholinergic properties of diphenhydramine, which block the action of acetylcholine, a crucial neurotransmitter involved in memory and learning, may contribute to significant cognitive decline over time. This revelation prompts a critical evaluation of the risks and benefits associated with these seemingly harmless OTC drugs.
Dr. Malaz Boustani, a research scientist specializing in aging and brain health at the Regenstrief Institute, emphasized the potential risks associated with diphenhydramine. “There’s enough data to suggest that you should be concerned about using these medications on a regular basis,” Boustani stated. He noted that while occasional use may not pose a significant threat, chronic or frequent reliance on diphenhydramine-containing products could have detrimental effects on cognitive function, especially in vulnerable populations such as older adults.
The concerns surrounding diphenhydramine are not new, as previous studies have explored the link between anticholinergic drugs and cognitive impairment. However, recent research has provided further insights into the specific mechanisms by which diphenhydramine may affect brain health and the extent of the associated risks. This has led to renewed calls for greater awareness among consumers and healthcare providers regarding the potential dangers of prolonged use.
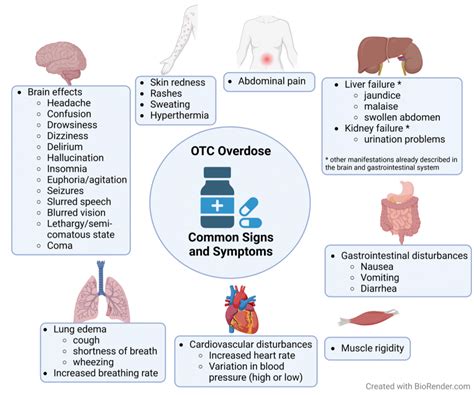
The potential risks of diphenhydramine stem from its anticholinergic properties. Acetylcholine is a neurotransmitter vital for various brain functions, including memory, learning, and attention. Anticholinergic drugs like diphenhydramine block the effects of acetylcholine, which can lead to a range of side effects, such as dry mouth, blurred vision, constipation, and urinary retention. While these side effects are often temporary and mild, long-term anticholinergic use has been linked to more severe consequences, including cognitive decline and an increased risk of dementia.
Several studies have investigated the association between anticholinergic drug use and cognitive impairment. A landmark study published in JAMA Internal Medicine in 2015 found a significant association between cumulative anticholinergic exposure and an increased risk of dementia. The study, which followed nearly 3,500 older adults for an average of seven years, found that those who took higher doses of anticholinergic drugs were more likely to develop dementia than those who took lower doses or did not take these medications at all.
Another study published in the British Medical Journal in 2018 examined the association between anticholinergic drug use and the incidence of dementia in a large cohort of older adults in the United Kingdom. The study found that long-term use of anticholinergic drugs, including diphenhydramine, was associated with a significantly increased risk of dementia, with the risk increasing with higher doses and longer duration of use.
These findings have prompted healthcare professionals to urge caution when prescribing or recommending diphenhydramine-containing medications, particularly for older adults. The American Geriatrics Society has included diphenhydramine on its Beers List, a list of medications that are potentially inappropriate for use in older adults due to their high risk of adverse effects.
The risks associated with diphenhydramine are particularly concerning for older adults because they are more susceptible to the drug’s anticholinergic effects. As people age, their brains become more sensitive to the effects of anticholinergic drugs, and they may experience more pronounced cognitive side effects. Additionally, older adults are more likely to be taking other medications that also have anticholinergic properties, which can increase their overall anticholinergic burden and further elevate their risk of cognitive impairment.
The increasing prevalence of dementia and Alzheimer’s disease globally underscores the importance of identifying and mitigating modifiable risk factors for cognitive decline. With millions of people relying on OTC medications containing diphenhydramine, the potential impact on public health is significant. It is crucial for individuals to be aware of the risks associated with these medications and to discuss alternative treatment options with their healthcare providers.
While occasional use of diphenhydramine may be acceptable for some individuals, experts recommend exploring alternative strategies for managing allergies, insomnia, and cold symptoms. For allergies, non-sedating antihistamines such as loratadine (Claritin) or cetirizine (Zyrtec) may be preferable. These medications have a lower risk of anticholinergic side effects and are less likely to cause cognitive impairment. For insomnia, behavioral therapies such as cognitive behavioral therapy for insomnia (CBT-I) can be effective in improving sleep quality without the need for medication. Lifestyle modifications such as establishing a regular sleep schedule, creating a relaxing bedtime routine, and avoiding caffeine and alcohol before bed can also help improve sleep.
The potential cognitive risks associated with diphenhydramine extend beyond older adults. Although older individuals are more vulnerable, prolonged exposure to anticholinergic drugs can affect cognitive function in younger populations as well. Studies have indicated that even short-term use of anticholinergic medications can impair memory, attention, and executive function in younger adults. Therefore, it is essential for individuals of all ages to be mindful of the potential risks and to use diphenhydramine-containing medications judiciously.
One of the challenges in assessing the risks of diphenhydramine is that it is readily available over the counter, without the need for a prescription. This means that many people may be using these medications without the knowledge or guidance of a healthcare provider. It is crucial for consumers to carefully read the labels of OTC medications and to be aware of the active ingredients and potential side effects. If you have any concerns about the safety of a medication, it is always best to consult with a healthcare professional.
Another challenge is that diphenhydramine is often combined with other medications in OTC products, such as cold and flu remedies. This can make it difficult for consumers to determine whether they are taking diphenhydramine and to assess their overall anticholinergic burden. It is essential to carefully review the ingredients of all medications you are taking and to be aware of the potential interactions and side effects.
Healthcare providers also play a crucial role in educating patients about the risks of diphenhydramine and in recommending alternative treatment options. Doctors and pharmacists should routinely screen patients for anticholinergic drug use, particularly older adults, and should consider deprescribing these medications when appropriate. Deprescribing involves gradually reducing or discontinuing medications that are no longer necessary or that pose a significant risk of adverse effects.
The findings regarding diphenhydramine highlight the importance of medication safety and the need for ongoing research to better understand the long-term effects of commonly used drugs. As the population ages, it is increasingly important to identify and mitigate risk factors for cognitive decline and to promote strategies for maintaining brain health throughout life.
In conclusion, the emerging evidence linking diphenhydramine to potential brain health risks underscores the need for greater awareness among consumers and healthcare providers. While occasional use may not pose a significant threat, chronic or frequent reliance on diphenhydramine-containing products could have detrimental effects on cognitive function, particularly in older adults. By exploring alternative treatment options and working closely with healthcare professionals, individuals can make informed decisions about their medication use and protect their long-term brain health.
The ongoing research emphasizes the need for a more comprehensive approach to medication safety. This includes increased awareness campaigns to educate the public about the potential risks associated with common OTC drugs, enhanced screening protocols for healthcare providers to identify individuals at risk, and the development of safer alternatives for managing allergies, insomnia, and other common ailments.
Furthermore, it is crucial to promote healthy aging strategies that can help to maintain cognitive function and reduce the risk of dementia. These strategies include regular physical exercise, a healthy diet, social engagement, and cognitive stimulation. By adopting a holistic approach to health and wellness, individuals can empower themselves to protect their brain health and to live longer, healthier lives.
Frequently Asked Questions (FAQ)
1. What is diphenhydramine, and where is it commonly found?
Diphenhydramine is an antihistamine medication used to relieve symptoms of allergies, hay fever, and the common cold. It works by blocking histamine, a natural substance in the body that causes allergic symptoms. It also has sedative properties, making it useful as a sleep aid. Diphenhydramine is commonly found in over-the-counter (OTC) medications such as:
- Allergy medications: Benadryl Allergy, some generic allergy tablets
- Sleep aids: Tylenol PM, Unisom SleepGels (containing diphenhydramine), ZzzQuil
- Cold and cough medications: Some combination cold and cough remedies
It is crucial to read the labels of OTC medications carefully to identify whether they contain diphenhydramine as an active ingredient.
2. What are the potential risks of taking medications containing diphenhydramine?
The primary concern with diphenhydramine is its anticholinergic properties. Anticholinergics block the action of acetylcholine, a neurotransmitter vital for memory, learning, and other cognitive functions. Potential risks associated with diphenhydramine use include:
- Cognitive impairment: Long-term use may contribute to memory problems, difficulty concentrating, and reduced overall cognitive function.
- Increased risk of dementia: Studies have linked chronic anticholinergic use to a higher risk of developing dementia, particularly in older adults.
- Side effects: Common side effects include dry mouth, blurred vision, constipation, urinary retention, and drowsiness. These side effects can be more pronounced in older adults.
- Falls: Due to its sedative effects and potential for dizziness, diphenhydramine can increase the risk of falls, especially in elderly individuals.
While occasional use might not pose significant risks, regular or long-term use should be approached with caution, particularly in older adults or individuals with pre-existing cognitive issues.
3. Who is most at risk from the potential cognitive side effects of diphenhydramine?
While anyone taking diphenhydramine can experience side effects, certain populations are at a higher risk:
- Older adults: The aging brain is more sensitive to the effects of anticholinergic drugs. Older adults are also more likely to be taking other medications with anticholinergic properties, increasing their overall “anticholinergic burden.”
- Individuals with pre-existing cognitive impairment: Those with mild cognitive impairment (MCI) or early stages of dementia may experience a faster decline in cognitive function with anticholinergic use.
- People taking multiple anticholinergic medications: Combining diphenhydramine with other drugs that have anticholinergic effects (e.g., some antidepressants, bladder control medications) can significantly increase the risk of cognitive problems.
- Individuals with certain medical conditions: People with conditions like glaucoma or prostate enlargement should use diphenhydramine with caution, as it can exacerbate these conditions.
4. What are some alternatives to diphenhydramine for allergies and sleep problems?
There are several alternatives to diphenhydramine for managing allergies and sleep problems, many of which have a lower risk of anticholinergic side effects:
- For allergies:
- Non-sedating antihistamines: Loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are less likely to cause drowsiness and cognitive impairment.
- Nasal corticosteroids: Fluticasone (Flonase), budesonide (Rhinocort), and triamcinolone (Nasacort) can effectively reduce nasal congestion and allergy symptoms.
- Saline nasal rinses: Help to clear nasal passages and relieve congestion.
- For sleep problems:
- Cognitive Behavioral Therapy for Insomnia (CBT-I): A structured therapy that addresses the underlying causes of insomnia.
- Melatonin: A natural hormone that regulates sleep-wake cycles.
- Good sleep hygiene: Establishing a regular sleep schedule, creating a relaxing bedtime routine, avoiding caffeine and alcohol before bed, and ensuring a comfortable sleep environment.
- Herbal remedies: Some people find relief with chamomile tea, valerian root, or lavender. However, consult with a healthcare provider before using herbal remedies, as they can interact with other medications.
It’s crucial to consult with a healthcare provider to determine the most appropriate alternative based on individual needs and medical history.
5. What should I do if I am currently taking medications containing diphenhydramine?
If you are currently taking medications containing diphenhydramine, consider the following steps:
- Consult with your healthcare provider: Discuss your medication use with your doctor or pharmacist. They can assess your individual risk factors, review your medication list for potential interactions, and recommend safer alternatives.
- Don’t stop abruptly: Do not suddenly stop taking diphenhydramine-containing medications, especially if you have been taking them regularly for a long time. Abrupt cessation can lead to withdrawal symptoms. Work with your healthcare provider to gradually reduce your dose if appropriate.
- Explore alternative treatments: Discuss non-pharmacological approaches and alternative medications with your doctor to manage your symptoms without relying on diphenhydramine.
- Monitor for cognitive changes: Pay attention to any changes in your memory, concentration, or overall cognitive function. Report any concerns to your healthcare provider.
- Read medication labels carefully: Always read the labels of OTC medications to identify active ingredients and potential side effects. Be aware of the anticholinergic effects of different drugs.
- Consider a medication review: Ask your healthcare provider to conduct a comprehensive medication review to identify any potentially problematic medications and to ensure that you are taking the most appropriate and safest medications for your conditions.
Expanded Context and In-Depth Analysis
The resurgence of concern surrounding diphenhydramine highlights a broader issue in healthcare: the underestimation of risks associated with seemingly innocuous over-the-counter medications. The ease of access and widespread availability of these drugs often lull individuals into a false sense of security, leading to chronic use without adequate awareness of potential long-term consequences. This situation is further compounded by aggressive marketing tactics that often downplay potential risks while emphasizing immediate symptom relief.
The specific mechanism by which diphenhydramine exerts its detrimental effects on brain health involves the disruption of cholinergic neurotransmission. Acetylcholine is a crucial neurotransmitter involved in a variety of cognitive processes, including memory formation, attention, and learning. By blocking acetylcholine receptors, diphenhydramine interferes with these processes, leading to cognitive impairment. The severity of cognitive effects can vary depending on factors such as dosage, duration of use, individual susceptibility, and the presence of other medical conditions.
The cumulative anticholinergic burden is a significant factor contributing to the risk of cognitive decline. Many medications, both prescription and over-the-counter, possess anticholinergic properties. When individuals take multiple medications with these properties, the combined effect can overwhelm the cholinergic system, leading to more pronounced cognitive impairment. Healthcare providers should routinely assess patients’ anticholinergic burden and consider deprescribing medications that are no longer necessary or that pose a high risk of adverse effects.
The implications of this research extend beyond individual health and have significant public health ramifications. As the global population ages, the prevalence of dementia is expected to increase dramatically. Identifying and mitigating modifiable risk factors, such as anticholinergic drug use, is crucial for reducing the burden of dementia on individuals, families, and healthcare systems.
Public health initiatives should focus on raising awareness about the potential risks of diphenhydramine and other anticholinergic drugs. This can be achieved through educational campaigns, public service announcements, and enhanced labeling requirements for OTC medications. Healthcare providers should also play a more proactive role in educating patients about medication safety and in recommending alternative treatment options.
Furthermore, research efforts should be directed towards developing safer and more effective alternatives for managing allergies, insomnia, and other common ailments. This includes exploring non-pharmacological approaches, such as behavioral therapies and lifestyle modifications, as well as developing new medications with fewer anticholinergic side effects.
The ethical dimensions of this issue also warrant consideration. Pharmaceutical companies have a responsibility to ensure that their products are safe and effective and that consumers are adequately informed about potential risks. Healthcare providers have a duty to provide patients with accurate and unbiased information about medications and to help them make informed decisions about their healthcare. Consumers have a responsibility to educate themselves about the medications they are taking and to discuss any concerns with their healthcare providers.
The challenge lies in balancing the immediate benefits of diphenhydramine in alleviating symptoms with the potential long-term risks to brain health. Occasional use of diphenhydramine may be appropriate for some individuals, but chronic or frequent use should be approached with caution, particularly in vulnerable populations such as older adults. By promoting greater awareness, fostering open communication between patients and healthcare providers, and investing in research and innovation, we can mitigate the risks associated with diphenhydramine and protect the cognitive health of individuals and communities.
The long-term societal costs associated with dementia are substantial, including healthcare expenses, long-term care costs, and lost productivity. Investing in preventive strategies, such as reducing anticholinergic drug use, can yield significant economic benefits by delaying the onset of dementia and improving the quality of life for individuals affected by cognitive decline.
Moreover, the regulatory framework governing OTC medications should be re-evaluated to ensure that these drugs are subject to appropriate levels of scrutiny and oversight. This includes requiring more comprehensive labeling, conducting post-market surveillance to monitor for adverse effects, and providing clear guidance to consumers about safe and effective use.
The issue of diphenhydramine and brain health underscores the complex interplay between medication use, aging, and cognitive function. By adopting a multidisciplinary approach that integrates research, education, clinical practice, and public policy, we can address this challenge effectively and promote healthy aging for all. The focus should be on empowering individuals to make informed decisions about their healthcare, supporting healthcare providers in providing evidence-based care, and creating a healthcare system that prioritizes medication safety and brain health. The overall goal is to ensure that the benefits of medications outweigh the risks and that individuals can maintain cognitive function and quality of life throughout their lifespan.